How can we make psychotherapy supervision more effective?
Last updated on 11th October 2018
All counsellors & psychotherapists in the UK need to have regular supervision if they want to maintain their professional accreditation. A central reason for this is to support therapists in being as helpful as possible for their clients. Unfortunately current approaches to supervision don't seem to do this particularly well. In a recent issue of the Cognitive Behavior Therapy journal, Alfonsson et al in their article "The effects of clinical supervision on supervisees and patients in cognitive behavioral therapy: a systematic review" clearly state "No study could show benefits from supervision for patients." And this depressing conclusion simply affirms what previous research has already highlighted for psychotherapy more generally ... see "Supervisor variance in psychotherapy outcome in routine practice" and "Does psychotherapy supervision contribute to patient outcomes? Considering thirty years of research", with the latter paper commenting "We do not seem to be any more able to say now (as opposed to 30 years ago) that psychotherapy supervision contributes to patient outcome."
Wow ... this is pretty damning. What on earth can be done to make supervision more effective? Here are three research-based suggestions:
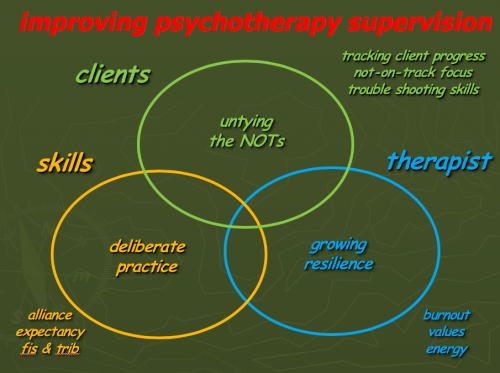
(This slide is downloadable by clicking here)
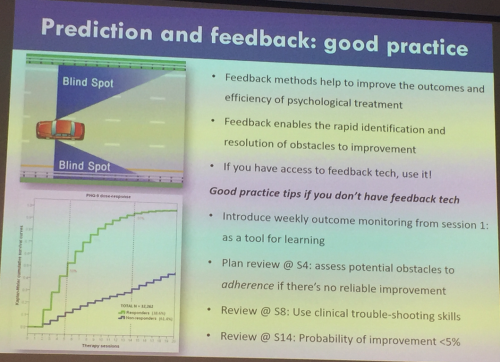
Taking these three areas in turn ... one obvious option to explore is better identification and trouble-shooting for the 10% or so of our clients who respond poorly. I have written extensively about this in many blog posts over the last ten or so years ... click, for example, on this website's tags for feedback and effectiveness. The recent Lancet Psychiatry paper "Feedback-informed treatment versus usual psychological treatment for depression and anxiety: a multisite, open-label, cluster randomised controlled trial" makes the argument for this stronger still. And this slide from a workshop I went to last month with Jamie Delgadillo, a main author of the Lancet paper, clarifies this further:
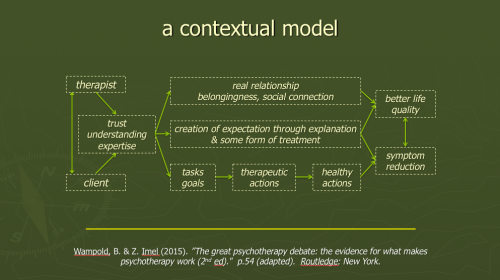
A second area to consider is skills improvement through 'deliberate practice'. What skills are worth focusing on in supervision and how can we best improve them? Well obvious questions to ask are "What therapist-related factors does research show make a difference to the effectiveness of therapy?" and "Can supervision usefully target these factors?" Here's a diagram adapted from Bruce Wampold & Zac Imel's fascinating book "The great psychotherapy debate".

(This slide & the one on Bruce Wampold's contextual model are downloadable by clicking here)
As you can see from the diagram, it makes sense to explore targeting therapist relational abilities and alliance factors. The effect size estimates on this chart are mostly taken from relevant chapters of John Norcross's excellent volume "Psychotherapy relationships that work". Making this latter book even more valuable, the various edited chapters typically end with specific suggestions for how therapists can apply the research findings in their work. Bruce Wampold's 'contextual model' of psychotherapy provides a helpful framework for these findings:
As an aside, I was at a one-day seminar with Bruce Wampold in May of this year and he made a fascinating throw-away comment about Tim Anderson’s 2009 study "Therapist effects: facilitative interpersonal skills as a predictor of therapist success", describing it as “The most informative psychotherapy study ever conducted.” Anderson's scoring manual for therapist 'facilitative interpersonal skills' interestingly looks at eight abilities: verbal fluency, hope & positive expectations, persuasiveness, emotional expression, warmth/acceptance/understanding, empathy, alliance bond capacity, and alliance rupture-repair responsiveness. There is a fair amount of overlap here with the nine group discussion qualities assessed in the intriguing, related research by Schöttke et al ... "Predicting psychotherapy outcome based on therapist interpersonal skills: A five-year longitudinal study of a therapist assessment protocol" ... clarity of expression, ability to present own ideas in a clear & convincing manner, capacity for careful & active listening, empathy/ability to accurately perceive the emotions of others, general behaviour towards others, response to contrary opinions, response to feedback about own behaviour (2 components), and ability & willingness to engage with & refine the ideas of other group members. You can find out more about the therapist qualities associated with improved client outcomes by clicking either/both effectiveness and psychotherapists in this website's tag cloud.
As a psychotherapist & doctor myself, I think health professionals sometimes emphasise empathy & compassion (which I hasten to add, I think are hugely important) ... at the expense of confidence & hope. It's intriguing how both Anderson and Schottke highlight the relevance to improved client outcomes of verbal fluency, hope & positive expectations, persuasiveness, clarity of expression and ability to present ideas in a clear & convincing manner (as well as response to contrary opinions). Fascinating. It reminds me of Jerome Frank classic 1960's book "Persuasion and healing", Tom Borkovec's more recent research, for example on "Psychometric propeties of the credibility/expectancy questionnaire", and more recently still Winfried Rief's expectancy intervention model described (in English) in "Erwartungsfokussierte psychotherapeutische interventionen".
And this skills-building area is not one that is typically focused on in routine supervision. It is likely to be served much better by including approaches like role-play, responses to pre-prepared challenging film clips, and other methods highlighted, for example, in Anders Ericsson's recent book "Peak: How all of us can achieve extraordinary things" rather than focusing on intellectually interesting but practically unproductive approaches like general discussion. Daryl Chow and Scott Miller have produced an intriguing 8-page "Taxonomy of deliberate practice activiities in psychotherapy" covering five domains - structure, hope & expectancy, working alliance, client factors & therapist factors (with relevant questions to ask oneself in each domain) - which (along with ideas from Norcross's book "Psychotherapy relationships that work") could be of particular use to attend to when focusing on skills-building in supervision.
And the third research-based suggestion I have for making supervision more effective is to monitor & respond to issues around therapist resilience & burnout. This year's important paper "Associations between therapists' occupational burnout and their patients' depression and anxiety treatment outcomes" commented "Occupational burnout is common in mental health professionals, but its impact on patient outcomes is as yet uncertain. This study aimed to investigate associations between therapist-level burnout and patient-level treatment outcomes after psychological therapy." The authors used the Oldenburg Burnout Inventory (OLBI) and the Job Satisfaction Scale (JDSS) and found that "Higher therapist OLBI-Disengagement and JDSS scores were significantly associated with poorer treatment outcomes, explaining between 31% and 39% of the TE (therapists' effects) estimate. Higher OLBI scores were also correlated with lower job satisfaction ratings. Conclusions: Therapist burnout has a negative impact on treatment outcomes and could be the target of future preventive and remedial action." Here is freely downloadable copy of the OLBI as a Word doc and as a PDF file - the researchers commented “Therapists are identified as having low, medium or high OLBI-D scores, based on scores above or below 1 standard deviation of the mean (M = 2.15, SD = 0.52; ≤1.62 = low, 1.63 to 2.67 = medium, ≥2.68 = high).” It's worth noting that a major review published this year - "Personal risk factors associated with burnout among psychotherapists: A systematic review of the literature" - reported that "Over half of sampled psychotherapists reported moderate-high levels of burnout" and a recent UK-based survey - "Predictors of emotional exhaustion, disengagement and burnout among Improving Access to Psychological Therapies (IAPT) practitioners" - reported even worse findings. Intriguingly this latter study reported "(higher) hours of clinical supervision predicted lower odds of burnout".
So to sum up ... research clearly suggests that most current approaches to psychotherapy & counselling supervision seem to make no significant difference to therapists' helpfulness for their clients. Reviewing recent literature on factors affecting outcomes highlights a variety of ways of improving this situation with three obvious areas being a focus on not-on-track cases, assessment & training in specific interpersonal & other skills, and monitoring & responding to therapist burnout/disengagement & job dissatisfaction.
